How often do you review a patient’s medication list and see a weight loss medication included, yet the patient still appears overweight, followed by the inevitable question: Why isn’t this working? What am I doing wrong? What else should I be doing?
That scenario has become increasingly common across outpatient clinics, specialty practices, telehealth visits, and follow-up encounters. Weight-loss medications are now routinely listed on medication lists, but their presence alone does not guarantee visible or sustained results.
For nurses, these are the moments that should shift the conversation away from medication safety and toward eating patterns, physical activity, sleep, stress, and long-term sustainability.
But this is where many nurses feel the disconnect.
What Education Do Patients Need Beyond Weight Loss Medication?
Patients using weight loss medication need education beyond dosing and side effects. Nurses should address nutrition quality, protein intake, strength training, sleep habits, stress management, and behavior change to support sustainable results and prevent muscle loss.
Where Nursing Education Ends and Patient Expectations Begin
Nurses are well-trained to discuss medications. Drug classifications, mechanisms of action, dosing, contraindications, side effects, and monitoring are core components of nursing education. When weight loss medications entered routine care, nurses were prepared to approach them through this familiar pharmacologic lens.
What most nurses are not trained to discuss are the other factors that determine whether weight loss actually occurs.
Weight loss medications can suppress appetite and reduce intake, but they do not replace the body’s need for adequate nutrition, muscle preservation, physical activity, sleep, stress regulation, and behavior change. These are the areas patients struggle with most and often expect nurses to help clarify.
When patients ask why a weight-loss medication is not working, the first question is usually about the dose. They want to know whether the dose should be increased or changed. What is often missing from these conversations is an understanding of what else influences outcomes. Patients may not realize that nutritional adequacy, muscle loss, exercise type, sleep, stress, and recovery play major roles in whether weight loss occurs. This places nurses in a critical position, not only to respond to what patients ask, but also to identify and address the factors patients do not yet know to question. Most nurses were never formally educated to do this.
Nutrition and Macros: Beyond “Eat Less”
Nutrition conversations about weight loss can quickly become confusing. Many patients believe that eating as little as possible will lead to better results. In reality, when calorie intake drops too low, the body pulls energy from both fat and muscle.
Muscle loss leads to weakness, fatigue, and stalled progress. This is why protein often comes up in the discussion, not because it is the only nutrient that matters, but because inadequate protein accelerates muscle loss during calorie restriction. This relationship is rarely taught outside of critical illness or inpatient care, leaving many nurses without a framework to explain it in outpatient weight loss conversations.
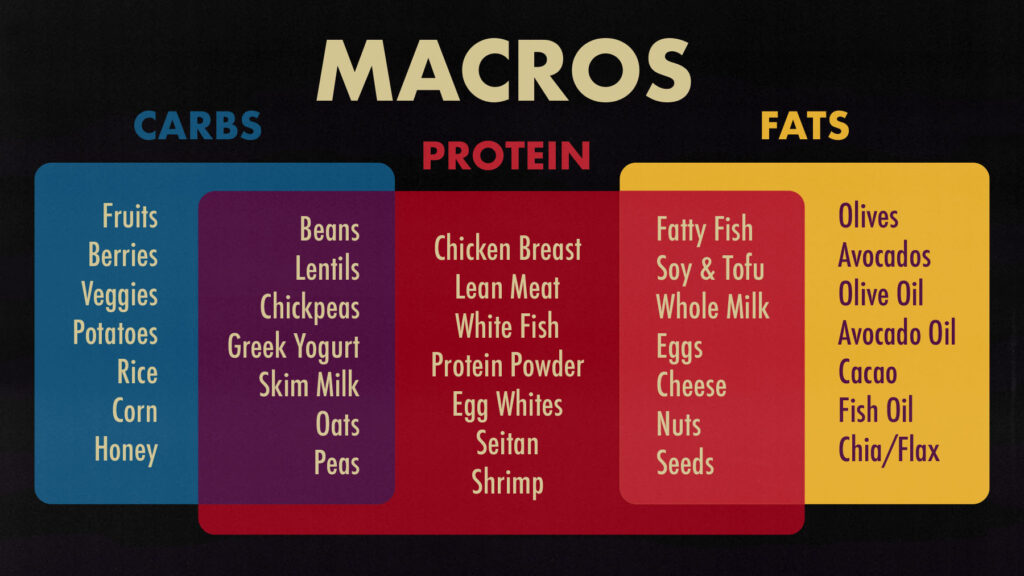
Patients also ask about carbohydrates and fats. Many assume carbohydrates should be avoided entirely or that fats are inherently harmful. Carbohydrates provide energy for daily activity and exercise, and overly restricting them can lead to fatigue, dizziness, and poor exercise tolerance. Dietary fats support hormone production, satiety, and absorption of fat-soluble vitamins, yet are often unnecessarily avoided.
Fiber is another frequent source of confusion. Patients may not understand the difference between starchy and non-starchy foods or how fiber supports fullness, gut health, and blood sugar regulation. Highly restrictive eating patterns, including many fad diets, can worsen fatigue and make weight loss harder to sustain, even with medication use.
Why Nurses Often Feel Hesitant Giving Nutrition Advice
Nursing education has traditionally approached nutrition through a disease-management lens. Renal diets, diabetic meal planning, cardiac sodium restriction, and fluid limitations are taught to protect patients with active illness. While essential, this framework often makes nurses cautious about giving broader dietary guidance.
As a result, many nurses feel more comfortable discussing what patients should avoid than how to fuel their bodies adequately for weight loss, muscle preservation, and activity. Weight loss medications have exposed this gap by shifting patient questions away from restriction and toward adequacy.
Fitness: Why Walking Alone May Not Be Enough
Patients commonly say, “I walk all the time. Why am I not losing weight?” Walking feels safe, familiar, and accessible, and it is often the primary activity patients are encouraged to do.
Walking supports cardiovascular health and daily movement, but walking alone may not be enough during weight loss. As body weight decreases, the body also loses muscle unless it is actively challenged. When muscle mass declines, the body burns fewer calories at rest, making continued weight loss harder over time.
In simple terms, less muscle means a slower engine.
Muscle loss does not only occur during illness. Adults begin to lose muscle mass gradually starting in their 30s and 40s, with the rate accelerating with age, inactivity, calorie restriction, and weight loss. Medication-assisted weight loss can speed this process when appetite is suppressed and strength training is absent.
Cardio, Strength, and Mobility
Healthcare has historically emphasized aerobic activity in patient education. This focus developed naturally from caring for acutely ill and chronically sick patients who lacked the strength or stability to safely perform resistance-based exercise. Walking and light cardio were often the most appropriate recommendations.
As a result, muscle-strengthening activity received less attention.
In the context of weight loss, this approach can be limiting. The American Heart Association recommends at least 150 minutes per week of moderate-intensity aerobic activity, along with muscle-strengthening activities on two or more days per week. Strength training preserves lean muscle mass, supports metabolism, protects bone density, and maintains functional independence as people age.
For patients using weight loss medications, strength training becomes especially important. Appetite suppression and reduced intake increase the risk of muscle loss. Without resistance exercise, patients may lose weight while becoming weaker and more fatigued, an outcome that is often unexpected and discouraging.
Stretching and mobility support recovery, comfort, and adherence. When stiffness or joint discomfort develops, patients are more likely to stop exercising altogether. Mobility work helps patients stay active consistently.
Sleep, Stress, and Mental Health Matter
Sleep plays a measurable role in weight loss. The American Heart Association recommends that adults get at least seven hours of sleep per night. Inadequate sleep increases ghrelin, which stimulates hunger, and decreases leptin, which signals fullness. This imbalance increases cravings and impairs insulin sensitivity.
Chronic stress elevates cortisol, which promotes fat storage and interferes with muscle recovery. Stress also disrupts sleep and reduces exercise tolerance, creating a cycle that undermines progress even when medications are used.
Mental health and mindset influence consistency and behavior change. When progress slows, patients often blame themselves. Nurses who understand these physiologic connections can reframe the experience and reduce shame.
A Call to Professional Growth
Patients often assume nurses are experts in weight loss, nutrition, and exercise. Nurses know that most formal training did not prepare them for this role.
This is not a failure of nursing. It reflects how nursing education evolved before medication-assisted weight loss became common. As these medications become routine, the expectation for nurses to provide practical, evidence-based guidance has grown.
Continuing Education Opportunity
To support nurses and healthcare professionals in closing these gaps, Nurse Approved invites you to join us for continuing education.
Weight Loss Education Nurses Need to Know for Their Patients: March 3, 2026
This program will cover nutrition and macronutrients; fitness, including cardio, strength, and stretching; sleep; stress; and the mental health components of behavior change, with practical guidance nurses can apply immediately.


