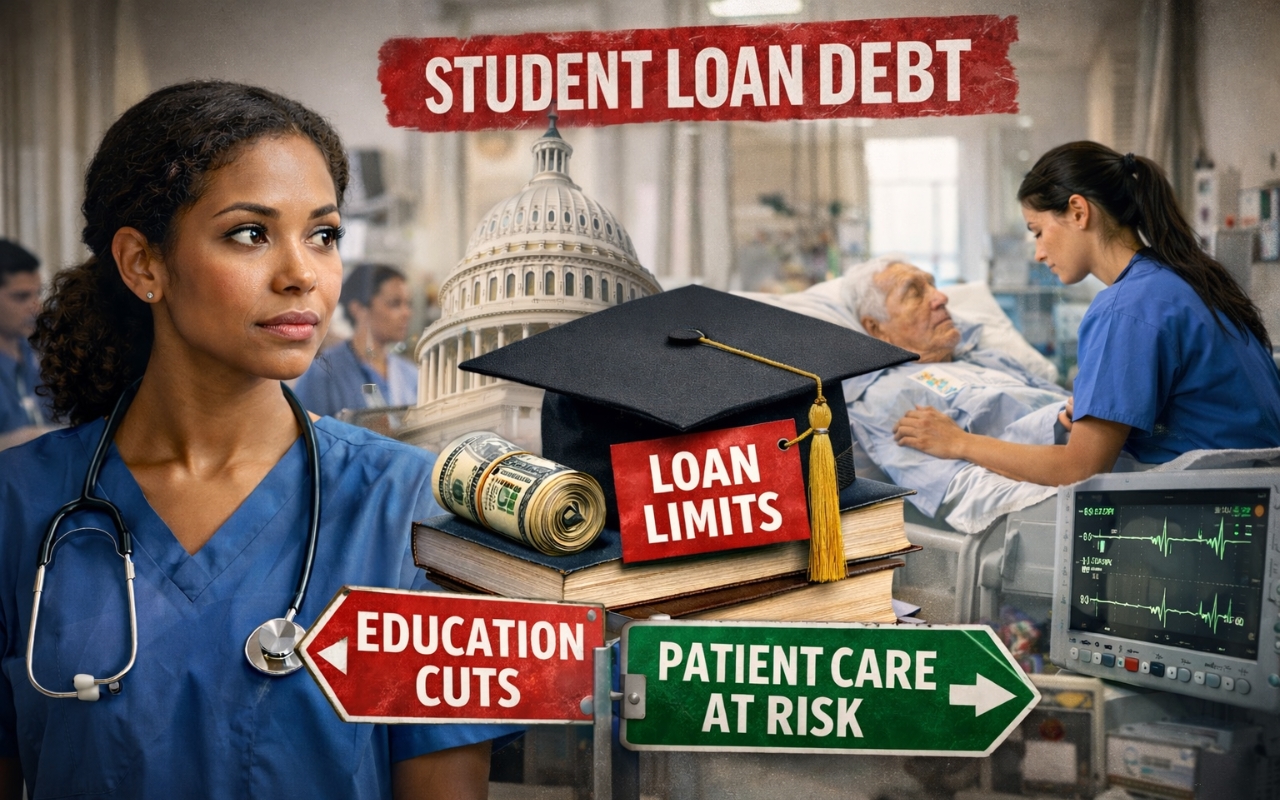
As the nation grapples with a growing shortage of healthcare workers, a new federal policy may make it even harder to train the next generation of nurse practitioners and nurse educators.
Recent changes from the U.S. Department of Education would reclassify advanced nursing programs as standard graduate degrees instead of professional degrees. That shift significantly limits how much federal loan money nursing students can access, potentially shrinking the pipeline of future providers at a time when demand is surging.
Valerie J. Fuller, PhD, DNP, AGACNP-BC, FNP-BC, FNAP, FAANP, president of the American Association of Nurse Practitioners (AANP), warns that the consequences could be far-reaching for nurses, patients, and the healthcare system.
What Do the New Federal Student Loan Rules Mean for Nursing Students?
The Department of Education’s proposed rule classifies nurse practitioner programs as the standard graduate category rather than as professional degree programs. This caps federal loan borrowing at $20,500 per year and $100,000 total, compared to $50,000 annually and $200,000 total for professional programs. According to AANP President Dr. Valerie Fuller, this change could prevent many nurses from affording advanced education and reduce patient access to care.
How the Rule Change Happened
Fuller explained that the policy stems from the passage of H.R. 1, which eliminated Grad PLUS loans and created new borrowing caps.
“For graduate students, the cap is $20,500 annually and $100,000 total. For professional students, it is $50,000 annually with a $200,000 aggregate,” Fuller said.
During the rulemaking process last fall, the Department of Education did not include nurse practitioner programs in the professional category. While nursing was not explicitly listed in the original 1965 Higher Education Act, Fuller noted the law was never meant to be restrictive.
“It actually says ‘but not limited to,’” she said. “Since that time, we have always been treated in the professional category and eligible for the higher loan amount.”
Under the new classification, nursing programs were officially placed in the graduate category, limiting how much students can borrow to complete their education.
“That is concerning because nurse practitioners are going to have less money than what they need to complete their education,” Fuller said.
The change also affects other critical healthcare fields, including physical therapy, occupational therapy, audiology, speech language pathology, and social work.
Why This Matters for Patients
Fuller emphasized the ripple effect this policy could have on patient care nationwide.
“We already have a number of nurse practitioners approaching retirement age,” she said. “If we have fewer students being educated and trained, we are going to have a reduced number of nurse practitioners entering practice.”
That reduction could mean longer wait times, limited access to primary care, fewer behavioral health services, and worsening provider shortages.
Recent data from the Medicare Payment Advisory Commission highlights the vital role nurse practitioners already play in care delivery.
According to Fuller, “Fifty-seven percent of Medicare beneficiaries receive their primary care services from a nurse practitioner or physician assistant. In rural areas, that number jumps to sixty-six percent.”
She added, “Patients will not have access to care. They will have longer wait times and have to travel greater distances.”
Financial Barriers Could Push Nurses Out
Fuller said the new borrowing caps create a major obstacle, especially since many advanced nursing programs cost well over $30,000 per year.
“If they cannot get enough money through federal loans, they will have to turn to private lenders,” she said. “Those loans have to be paid back while they are still in school, the interest rates are much higher, and some can be predatory.”
She also pointed out how trimester programs complicate the math.
“If you are capped at $20,500 annually, that will not cover three semesters. You are not even getting a full year of funding,” Fuller said.
Importantly, these are loans, not grants.
“This is not free money from the government. It is a loan that has to be paid back,” she said.
Impact on the Nursing Workforce Pipeline
Fuller warned that limiting access to graduate education could worsen existing shortages.
“Last year, the American Association of Colleges of Nursing reported that 65,000 qualified students were turned away from nursing programs because of faculty shortages,” she said.
Since nursing faculty must hold at least a master’s degree, barriers to graduate education will further shrink the educator workforce, worsening RN shortages and limiting future APRN numbers.
“Advanced practice nurses start as RNs. If there are fewer nurses in the pipeline, there are fewer APRNs too,” Fuller said.
Equity and Diversity at Risk
Fuller expressed concern about who will be most impacted by the policy.
“I worry most about students from low and middle-income backgrounds. They are going to get priced out of nursing,” she said.
She also emphasized the implications for diversity.
“Nursing is still a mostly white, female-dominated profession. We desperately need more diversity,” Fuller said. “This categorization will limit students from underrepresented backgrounds from entering nursing.”
That loss directly affects patient care.
“People often want to be cared for by someone who looks like them or is like them in some way,” she said. “We already have disparities in many communities.”
AANP’s Advocacy Efforts
AANP has been actively pushing back. Fuller said the organization submitted formal comments to the Department of Education last August and launched a nationwide letter-writing campaign to Congress.
“So many letters were sent that it prompted a bipartisan group of representatives to urge the Department of Education to change the rule,” she said.
The organization is also using its Advocacy Center, open to the public, to help individuals contact lawmakers.
“This is not a done deal yet,” Fuller emphasized. “The Department of Education will soon open a 30-day public comment period.”
Once it opens, AANP will urge nurses and the public to submit feedback directly to the Department of Education. The final rule is expected to take effect July 1, 2026.
Nurse Practitioners by the Numbers
Fuller underscored the scope of nurse practitioner impact.
“Last year, nurse practitioners performed almost a billion patient care visits,” she said.
“In 2024, there were 243,000 nurse practitioners billing Medicare. Eighty percent of nurse practitioners see Medicare patients.”
“These are some of our most vulnerable individuals,” she added.
Why Nursing Meets the Definition of a Professional Degree
Fuller pointed out that the Department of Education’s own definition supports nursing’s inclusion.
“A professional degree signifies completion of academic requirements for practice, advanced skill beyond a bachelor’s degree, and professional licensure,” she said. “Nurse practitioners meet every part of that definition.”
Looking Ahead as AANP Marks 40 Years
As AANP celebrates its 40th anniversary, Fuller said the organization remains focused on protecting the profession’s future.
“For forty years, AANP has been the voice of nurse practitioners,” she said. “We have worked to remove barriers and expand access to care.”
She added, “Over 100 million Americans still lack access to basic primary care. Nurse practitioners are the answer to that problem, but we need these loans to complete our education.”
How Nurses and the Public Can Get Involved
Fuller urged readers to follow AANP on social media and visit www.aanp.org, noting that the organization’s Advocacy Center will share timely updates when the public comment period opens and offer guidance on how to write letters to the Department of Education.
Her closing message emphasized what is at stake if these changes move forward.
“Less access to federal loans means fewer nurse practitioners. And ultimately, patients will pay the price with less access to care.”